Private Equity came for my wife’s psychiatric private practice EHR, Luminello. Luminello sold to SimplePractice, which is owned by EngageSmart, which is owned by Vista Equity Partners Management.
From the press release:
“Both SimplePractice and Luminello were founded by clinicians looking to simplify the business of running an independent solo or small group mental health practice,” said Ken Braslow, MD, Founder, Luminello.
“Today, we remain equally committed to removing the administrative burdens that practitioners face and look forward to combining the strength of our collective experience to serve even more practitioners and their patients.”
Apparently, Luminello’s “commitment” was worth $19.6 million.
In short order, SimplePractice announced they were shutting down Luminello.
In fact, Luminello is being shut down so fast that SimplePractice doesn’t yet have the features needed to run an actual medical practice. They’re pressuring docs to transition despite the reality that SimplePractice is currently mostly used by nonphysician therapists and is half-baked as an EHR: They don’t have labs! They don’t have snippets or dot-phrases! They don’t even have e-prescribe! (You get the idea.)
Communication about the transition has been generally confusing and poor, but here’s the fun daily DocuSign reminder that assumes you’ll take it on faith that SimplePractice is going to work for your practice and are coming along for the ride:
In typical tone-deaf private equity fashion, they’re happy to spend money upfront for a roll-up to buy (instead of earn) some growth but then completely botched the execution because they don’t actually know what they’re doing. Instead, they’d rather anger thousands of doctors by bullying them into switching to a product that literally can’t do many of the things their current offering does while pressuring them in the sleaziest ways possible.
Luminello is flawed, but it works worked. In the meantime, its customers are being told they only have until April to sign on to SimplePractice before their EHR stops working.
Meanwhile, the data export function the docs need to save their records (and, coincidentally, to transition to a different EHR) seems to be magically broken. Their patient information is being held hostage.
Just for fun, the entire lab-ordering tab has disappeared.
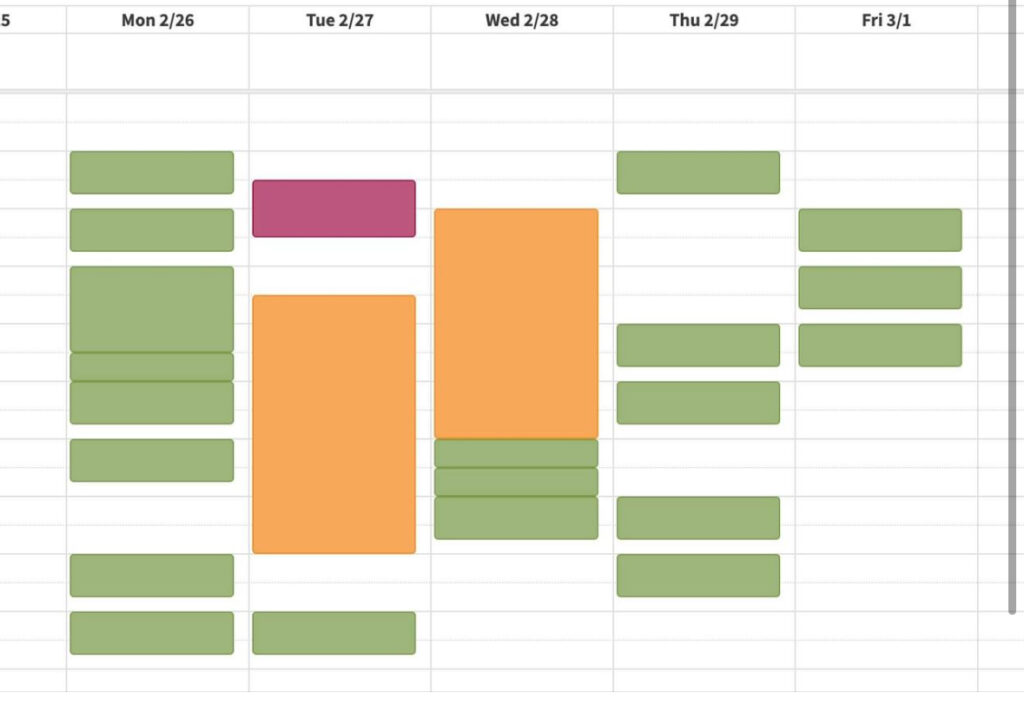
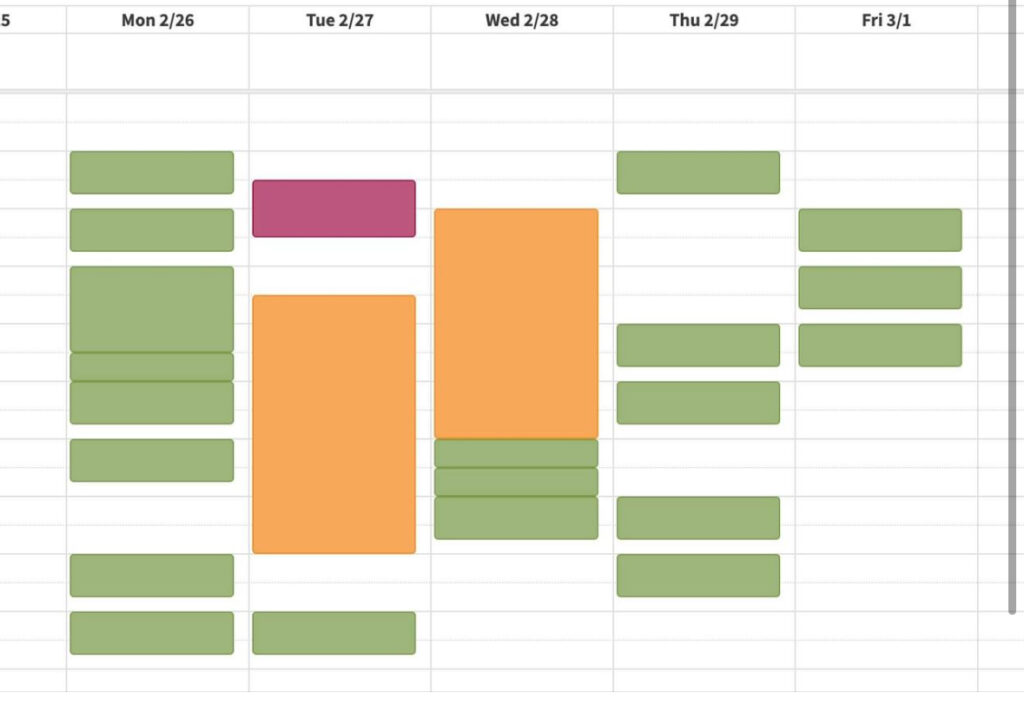
Starting a few days ago, for some users, the Luminello calendar began intermittently showing empty appointment slots:
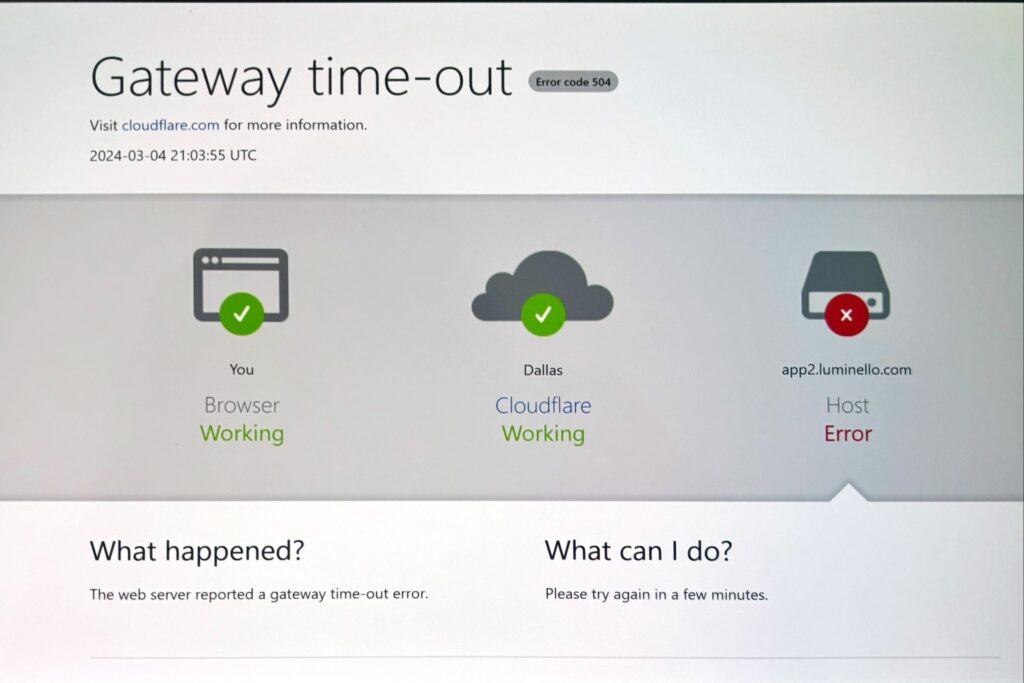
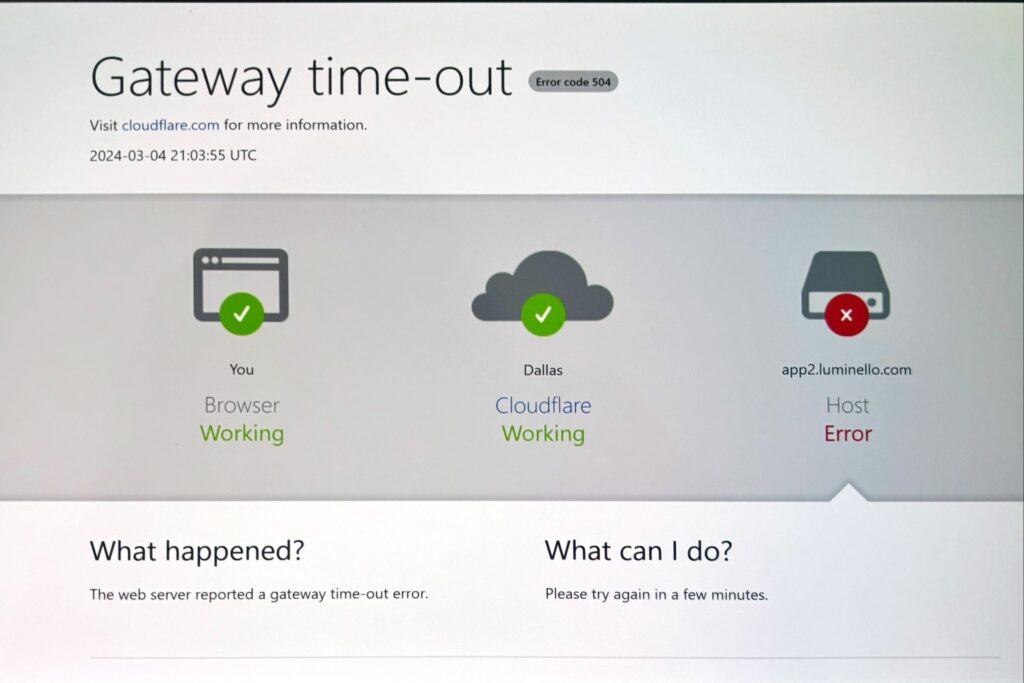
And, just today, the site began alternating between intermittently lagging into unusability and just flat-out crashing:
Now, why spend millions to basically buy customers and then immediately turn around and make all of their lives harder instead of just waiting a few more months until you have feature parity? Why not make switching an easy no-brainer upgrade?
Because, in my opinion, they don’t think it matters.
They don’t seem to care about their customers or about the patients (“clients” in SimplePractice parlance) their customers serve, and—most importantly—they’re relying on doctor’s learned helplessness: they assume a critical mass of physicians using Luminello—many in solo practice—are resigned to the enshittification of healthcare or too busy to actively pick something else.
I hope they’re wrong.